When we think about healthcare, we often picture hospitals, prescriptions, and surgeries. We think of doctors “fixing” us after something goes wrong. But a quiet revolution is happening in American medicine, shifting the focus from fixing problems to stopping them before they start. This is the domain of preventive medicine.
As healthcare costs continue to climb and chronic diseases become more common, the old model of waiting for sickness to strike is proving unsustainable. Preventive medicine offers a different path—one that prioritizes wellness, early detection, and long-term health maintenance. It is not just about avoiding the doctor; it is about engaging with healthcare in a smarter, more proactive way to live a longer, healthier life.
What Is Preventive Medicine?
At its core, preventive medicine is exactly what it sounds like: medical practices designed to ward off disease and injury. It is a proactive approach to patient care that focuses on maintaining health rather than just treating illness.
While traditional healthcare often operates on a reactive model—treating symptoms after they appear—preventive medicine is forward-looking. It asks, “What can we do today to ensure you don’t get sick tomorrow?” This shift from treatment-based care to prevention-based care transforms the patient experience. Instead of seeing a physician only during a crisis, patients partner with providers to manage risk factors like diet, exercise, and environmental exposures.
Why Preventive Medicine Matters in Modern Healthcare
The United States faces unique healthcare challenges that make prevention more critical than ever. Two major factors are driving this urgency: the rising tide of chronic disease and the skyrocketing cost of care.
Chronic diseases such as heart disease, cancer, and diabetes are the leading causes of death and disability in the U.S. According to the CDC, six in ten American adults have a chronic disease, and four in ten have two or more. Many of these conditions are preventable or manageable through lifestyle changes and early intervention. Without a strong focus on prevention, the burden of these diseases will continue to strain the healthcare system and reduce quality of life for millions.
Financially, the U.S. spends more on healthcare per capita than any other developed nation, yet health outcomes often lag behind. A significant portion of this spending goes toward treating advanced stages of preventable diseases. By catching issues early or preventing them entirely, the system can alleviate the massive financial pressure on families, insurers, and the government.
Types of Preventive Medicine
Preventive care isn’t a one-size-fits-all concept. It is generally categorized into three distinct levels, each targeting a different stage of health and disease.
Primary Prevention
Primary prevention aims to stop a disease or injury before it ever occurs. This is the most proactive form of healthcare. It includes:
- Vaccinations: Immunizing against infectious diseases like the flu, measles, or hepatitis.
- Lifestyle Interventions: Counseling on smoking cessation, nutrition, and exercise to prevent conditions like heart disease or lung cancer.
- Safety Measures: Promoting the use of seatbelts and bike helmets to prevent traumatic injuries.
Secondary Prevention
Secondary prevention focuses on early detection. The goal is to catch a disease in its earliest stages when it is most treatable, often before the patient notices any symptoms.
- Screenings: Mammograms for breast cancer, colonoscopies for colorectal cancer, and blood pressure checks for hypertension.
- Early Intervention: Starting low-dose medication for someone with elevated cholesterol to prevent a future heart attack.
Tertiary Prevention
Tertiary prevention is for patients who already have a diagnosed disease. The objective here is to manage the condition to prevent it from getting worse and to stop complications from developing.
- Rehabilitation: Physical therapy after a stroke to regain function.
- Chronic Disease Management: Regular check-ins and medication management for diabetics to prevent complications like nerve damage or kidney failure.
Common Preventive Healthcare Services in the USA
In the United States, accessing preventive care has become easier due to legislative changes like the Affordable Care Act (ACA), which requires most insurance plans to cover specific preventive services at no cost to the patient.
Annual Checkups: The yearly physical is the cornerstone of preventive health. It allows doctors to track changes in a patient’s health over time and update family history records.
Immunizations: From childhood vaccines to annual flu shots and shingles vaccines for seniors, immunizations act as a shield against preventable outbreaks.
Wellness Visits: For women, “well-woman” visits often include pap smears and bone density scans. For children, “well-child” visits track growth and developmental milestones to ensure they are on the right path.
Preventive Medicine and Chronic Disease Prevention
The battle against chronic disease is perhaps where preventive medicine shines brightest.
Heart Disease and Diabetes: These are two of the biggest killers in America, yet they are highly responsive to preventive measures. Regular blood work can identify pre-diabetes or high cholesterol years before a crisis occurs. With this data, patients can make dietary changes or start medications that drastically reduce the risk of heart attacks and strokes.
Obesity and Lifestyle Conditions: Obesity is a gateway to numerous other health issues, including joint problems and sleep apnea. Preventive medicine addresses this through nutritional counseling and weight management programs, treating obesity as a medical condition requiring support rather than just a willpower issue.
Role of Preventive Medicine in Public Health
Preventive medicine extends far beyond the individual doctor’s office; it plays a massive role in public health. When prevention strategies are applied at a population level, the results can be transformative.
Public health initiatives rely on preventive principles to protect communities. This includes ensuring clean water, managing sanitation, and running educational campaigns about the dangers of smoking or vaping.
Community and workplace programs also contribute significantly. For example, a city might invest in bike paths to encourage exercise, or a company might offer flu shot clinics in the breakroom. These broad strokes help improve health outcomes for thousands of people at once, reducing the overall strain on local hospitals and clinics.
Preventive Medicine and Healthcare Costs
There is a common saying: “An ounce of prevention is worth a pound of cure.” In the U.S. healthcare system, that pound of cure is incredibly expensive.
Treating advanced diseases requires surgeries, long hospital stays, and expensive specialty drugs. In contrast, the interventions used in preventive medicine—like a course of blood pressure medication or a consultation with a dietician—cost a fraction of that amount.
By intervening early, the system avoids expensive emergency room visits. For instance, managing a patient’s asthma through regular check-ups and inhalers is far cheaper (and safer) than treating a severe asthma attack in the ICU. While preventive care requires an upfront investment, the long-term savings for the healthcare system are substantial.
Technology’s Role in Preventive Healthcare
Technology is rapidly changing how we approach prevention, moving it from the clinic into our daily lives.
Wearables and Health Monitoring: Smartwatches and fitness trackers allow individuals to monitor their heart rate, sleep patterns, and activity levels in real-time. This data empowers patients to take charge of their health and provides doctors with a more complete picture of a patient’s lifestyle than a single office visit ever could.
Telehealth and Digital Screenings: Telehealth has removed barriers to care, making it easier for people in rural areas or with busy schedules to consult with physicians. Digital tools can now screen for mental health conditions or analyze skin lesions via smartphone cameras, making early detection more accessible than ever.
Preventive Medicine and Aging Populations
As the Baby Boomer generation ages, the U.S. population is getting older. Preventive medicine is essential for ensuring that living longer also means living better.
Healthy Aging Strategies: Prevention for seniors focuses on maintaining independence and quality of life. This includes fall prevention programs, strength training to prevent muscle loss, and cognitive exercises to maintain brain health.
Early Risk Identification: As we age, the risk for conditions like osteoporosis and dementia increases. Regular screenings allow for early management of these conditions, helping seniors avoid fractures and maintain mental clarity for as long as possible.
Barriers to Preventive Care Adoption
Despite the clear benefits, not everyone in the USA gets the preventive care they need. Several barriers stand in the way.
Access and Affordability: Even with insurance reforms, cost remains a barrier. High deductibles or copays for follow-up tests can deter people from seeking care. Furthermore, “medical deserts” in rural and low-income urban areas mean that for many, a doctor is simply too far away.
Awareness and Health Literacy: Many people simply don’t know which screenings they need or when they need them. Navigating the complex U.S. healthcare system requires a level of health literacy that not everyone possesses, leading to missed opportunities for early intervention.
Preventive Medicine in Employer-Sponsored Healthcare
Since many Americans get their health insurance through their jobs, employers play a pivotal role in preventive health.
Workplace Wellness Programs: Progressive companies are realizing that a healthy workforce is a productive one. They are implementing wellness programs that offer gym memberships, smoking cessation support, and stress management workshops.
Incentives for Preventive Care: Some employers offer financial incentives, such as lower insurance premiums or contributions to Health Savings Accounts (HSAs), for employees who complete their annual biometric screenings or health assessments. This gamification of health encourages employees to stay on top of their preventive needs.
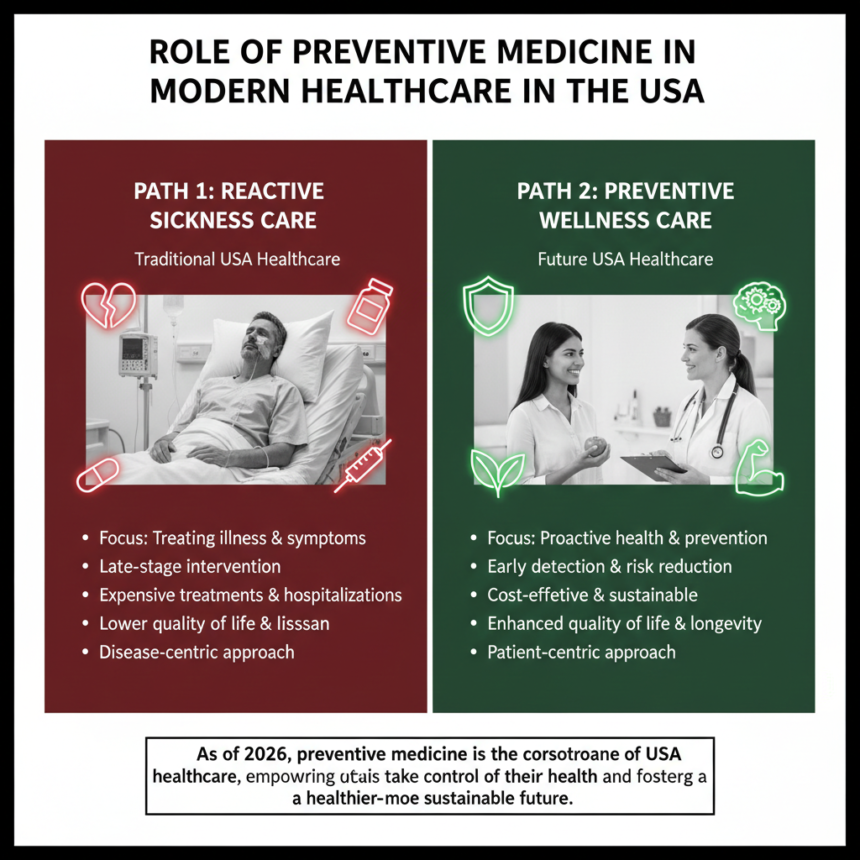
Preventive Medicine vs Reactive Healthcare Models
The tension between preventive and reactive models is the central conflict in modern healthcare.
The reactive model is familiar: you feel sick, you go to the doctor, you get treated. While necessary for acute injuries and infections, this model fails when applied to chronic lifestyle diseases. It is expensive and often results in poorer outcomes because the disease has had time to cause damage.
The preventive model flips the script. It is less dramatic but more effective. It requires patience and consistent engagement. When comparing outcomes, preventive models consistently lead to longer life expectancies and better quality of life. For the sustainability of the U.S. healthcare system, a shift toward prevention is not just a preference; it is a mathematical necessity.
Future of Preventive Medicine in the USA
The future of preventive medicine is personalized and precise. We are moving away from general guidelines based on age and toward strategies tailored to the individual.
Personalized Prevention Strategies: Advances in genomics will allow doctors to look at a patient’s DNA to understand their specific risks for diseases like cancer or Alzheimer’s. Prevention plans will be custom-built based on genetic markers.
Data-Driven Risk Prediction: Artificial Intelligence (AI) will play a massive role. By analyzing vast amounts of health data, AI will be able to predict who is at risk for certain conditions with incredible accuracy, allowing for interventions that are perfectly timed and highly effective.
Leading a Healthier Life
Preventive medicine represents a fundamental shift in how we view health. It empowers individuals to be the architects of their own well-being rather than passive recipients of care. By embracing screenings, vaccines, and healthy lifestyle choices, Americans can look forward to a future where healthcare is less about treating sickness and more about cultivating wellness.
Meta data
Meta title
The Role of Preventive Medicine in Modern US Healthcare
Meta description
Discover how preventive medicine is transforming US healthcare. Learn about the benefits of early detection, primary prevention, and proactive wellness.
FAQs – Preventive Medicine in the USA
What is preventive medicine in simple terms?
Preventive medicine refers to healthcare practices designed to prevent illness and disease before they happen, rather than treating them after you get sick. This includes check-ups, vaccines, and lifestyle advice.
Why is preventive care important?
It is important because it helps you live a longer, healthier life. By catching health issues early or preventing them entirely, you avoid the pain, stress, and high costs associated with severe chronic diseases.
Does preventive medicine lower healthcare costs?
Yes, in the long run. While there is a cost for screenings and check-ups, it is significantly cheaper than paying for emergency surgeries, hospitalizations, and long-term treatments for advanced diseases.
What preventive services are most important?
The most important services vary by age and gender, but generally include annual physicals, blood pressure checks, cholesterol screenings, recommended vaccinations, and cancer screenings like mammograms or colonoscopies.
Is preventive care covered by insurance in the USA?
Thanks to the Affordable Care Act (ACA), most private insurance plans and Medicaid expansion plans must cover a set of specific preventive services—like shots and screening tests—at no cost to you (no copayment or coinsurance).


Leave a Reply